
Feeling blue?
You’ve just given birth to a wonderful baby, and everyone’s ecstatic. Everyone, that is, except you. If this is supposed to be such a happy time, why do you feel so low?
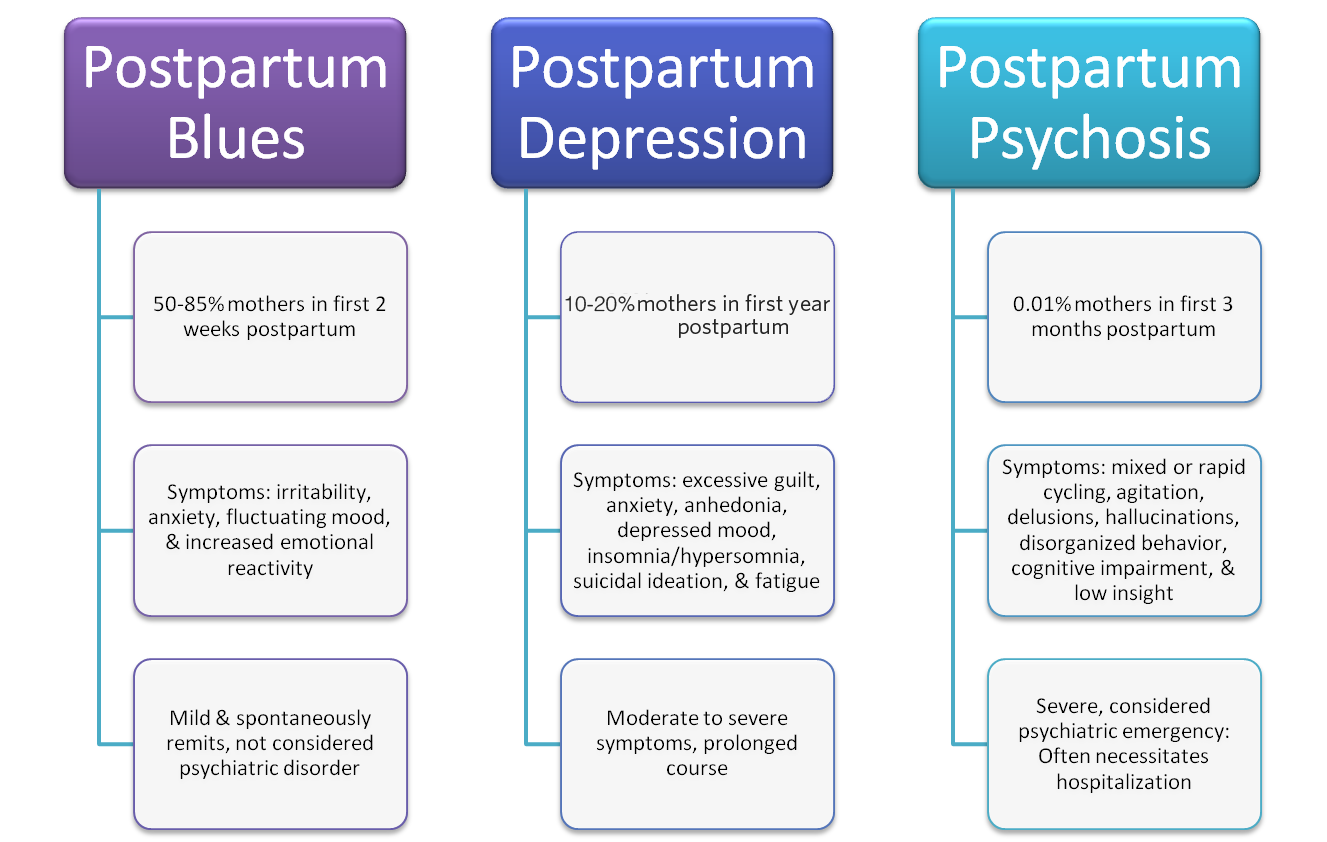
You’re not alone. Some degree of emotional vulnerability is natural and expected after childbirth. Up to 85% of new mothers experience the Baby Blues, and emotional reaction that begins a few days to a week after delivery and generally lasts no longer than two weeks. If you have the blues, you may be weepy, worried, and unable to sleep. You may also be irritable and moody.
Moms often feel better after getting some rest and a helping hand with the baby. But if your blues–or those of someone you love–have lasted more than two weeks, read on.
HMHB now offers Postpartum Depression Counseling!
HMHB now offers postpartum depression counseling services onsite at our downtown office. Don’t forget to take care of yourself during times of intense stress. Your mental health matters.
What causes depression after childbirth?
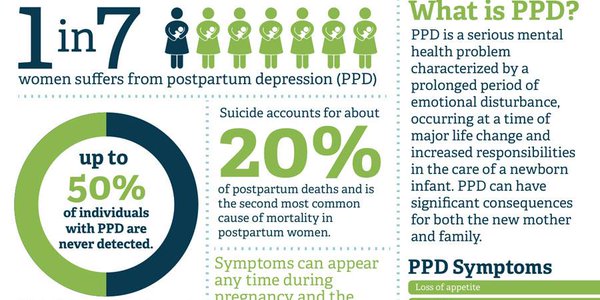
Experts agree that there’s no single cause, but rather a combination of hormonal, biochemical, environmental, psychological, and genetic factors. In all, about 10-20% of new mothers experience clinical depression, anxiety, or obsessive-compulsive disorder (OCD). Current research indicates that one of the strongest predictors of PPD is depression or anxiety during pregnancy.
Am I at risk for postpartum depression (PPD)?
Some women are more likely than others to get PPD. The strongest predictors of postpartum depression are:
- Bouts of intense depression or anxiety while you were pregnant, particularly in the third trimester.
- Prior history of depression or anxiety.
- Family history of depression or anxiety.
- Marital difficulties.
- Stressful life events such as financial problems or the loss of a job.
- Childcare stress.
- Inadequate social support.
- Having to care for a child with a difficult temperament.
- Low self-esteem.
Other less predictive risk factors include unplanned or unwanted pregnancy, being single, lower socioeconomic status, and postpartum blues.
Remember that these risk factors don’t actually cause PPD. Many women with a number of them never experience clinical depression, anxiety, or OCD. Others with just one risk factor, or even none, end up with a full-blown clinical condition.
Could I be suffering from postpartum depression (PPD)?
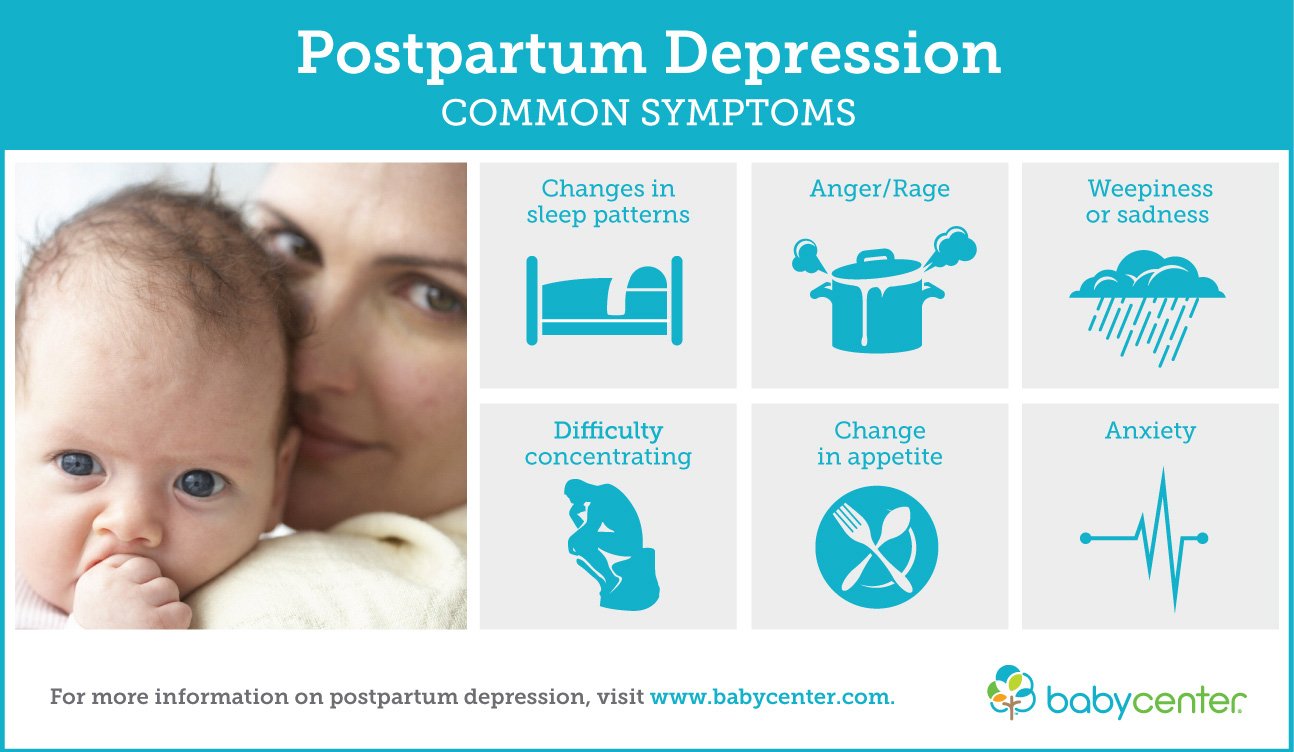
If you’re concerned, don’t wait until your next postpartum doctor visit–talk to your healthcare provider immediately. She can screen you for PPD and refer you to a counselor if needed. With PPD, the feelings of sadness can be extreme, last longer than two weeks, and may interfere with the ability to take care of yourself or your family. Because of the severity of the symptoms, PPD usually requires treatment.
Some women with PPD believe they can’t adequately care for, or may even harm, their baby. If you think you might hurt yourself or your baby, or if you feel incapable of caring for your newborn, seek professional help immediately. You are not alone; help is available!
What is postpartum anxiety?
If you’re having recurrent feelings of intense worry or panic, you may have postpartum anxiety disorder. Recent research has shown that about 10% of postpartum moms suffer from clinical anxiety.
Anxiety symptoms usually appear in the first two to three weeks after the birth of a baby, but may not reach a distressing level until several weeks later. There is some overlap between depression and anxiety, and some women have symptoms of both. Symptoms of anxiety and panic may include:
- Extreme anxiety or irritability
- Restlessness and agitation
- Shortness of breath
- Chest pains or discomfort
- Sensation of choking or smothering
- Dizziness
- Tingling in hands or feet
- Trembling and shaking
- Sweating
- Faintness
- Hot or cold flashes
- Fear of dying, of going crazy, or of losing control
Some women with postpartum anxiety have recurrent fears about harm coming to their children, other loved ones, or themselves. If you have these feelings, discuss them with your healthcare provider.
What is postpartum obsessive-compulsive disorder?
Postpartum OCD is characterized by persistent, recurring thoughts about intentional or accidental harm coming to the baby. The thoughts or images are often disturbing or violent, and arise spontaneously in the first couple of weeks after giving birth. They may include thoughts such as stabbing the baby with knives or putting the baby in the oven.
Like other OCD sufferers, women with postpartum OCD see danger everywhere and seek to avoid it through repetitive and ritualistic behaviors. They may hide the knives or avoid the kitchen in an effort to ward off thoughts of harming the baby. Some women may avoid basic care, refusing to bathe their baby out of fear of thoughts about death by drowning. Unlike women with postpartum psychosis (PPP), women with postpartum OCD are repulsed by these thoughts of harming their baby, and know not to act on them.
If you ever feel compelled to act on these thoughts, seek professional help immediately. You may have what’s known as postpartum psychosis, a severe yet rare illness characterized by hallucinations, bizarre thinking, paranoia, mania, delusions, and suicidal impulses. PPP requires immediate medical intervention due to the increased risk of suicide for the mother and harm to the baby.
What can I do to cope?
In addition to getting expert help from your healthcare team, here are some ways to take care of yourself when you’re dealing with postpartum depression, anxiety, or OCD:
- Be good to yourself.
Make sure your own basic needs are met. Try to sleep and eat well, and try not to feel guilty about the way you feel now. Just because you have PPD doesn’t mean you are a bad mother or don’t love your child. Once you feel better, these feelings will diminish.
- Don’t expect so much of yourself.
If you have clinical depression, anxiety, or OCD, it is enough just to get out of bed and face the day. Focus on taking good care of yourself. If you can do this each day, you’ll be doing well.
- Ask for support.
Part of being a good mother is knowing when to ask for help – so don’t be afraid to ask for it during this difficult time. Help comes in many forms, ranging from friends who cook meals and fold your laundry to therapy. You need support from others so you can get better.
- Share your feelings.
Tell someone you trust about how you feel. Call a sympathetic friend. Join a mothers’ group for support, or call our MothersCare line for support at: (808) 951-6660 or (888)951-6661. You may be surprised at how many women are experiencing similar feelings. If you have a supportive partner, make sure he or she knows what’s going on and how to help.
- Don’t neglect your “outside.”
Taking care of your physical self can sometimes help you feel better inside. Have your partner or a friend watch your baby so you can take a relaxing shower. Put on makeup if you usually wear it. Go on a shopping trip just for yourself and buy something new for your post-birth wardrobe. Wear a favorite outfit on especially difficult days to give yourself a boost.
- Get some rest.
The rigors of caring for a newborn 24/7 can leave you exhausted. Unfortunately, moms with postpartum clinical conditions often can’t sleep when they want to. But it’s still important to give yourself rest breaks, even if you just read a magazine or watch TV. Ask a relative or friend to watch your baby for an hour or so each day. If no one’s available, consider hiring a postpartum doula or a sitter experienced with newborns.
- Venture outdoors.
Put your baby in a stroller and take a walk around the block, or meet a friend at a nearby café. The fresh air, sunshine, and conversation will do you and your baby a world of good. If even a brief excursion is too much for you right now, then just go outside, close your eyes, take a deep breath, and sit in the sunshine for a few minutes. It will help.
- Slow down.
Your baby’s arrival is a good reason to take it easy. Resist the temptation to do the laundry while your baby sleeps, and let the rest of your chores wait. Have food delivered, or ask your partner to get takeout on the way home. Turn off the ringer on the phone when you’re trying to get the baby to sleep or when you’re finally sitting down for a much-needed break. If you’re on maternity leave, banish all thoughts of the work awaiting you at the office. Don’t worry – you’ll get back on track soon enough.
The Edinburgh Postpartum Depression Symptoms Quiz and Score Tool
This tool calculates your depression score in 10 questions.
Learn More

Sources
1) Postpartum Depression Facts, National Institute of Mental Health. Available at: https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml
2) Postpartum Depression FAQ, American College of Obstetricians and Gynecologists. Available at: https://www.acog.org/Patients/FAQs/Postpartum-Depression
3) Postpartum Depression Fact Sheet, PRAMS. Available at: http://health.hawaii.gov/mchb/files/2013/05/postpartum20101.pdf


